Understanding Coronary
Artery Disease
What
is coronary artery disease?
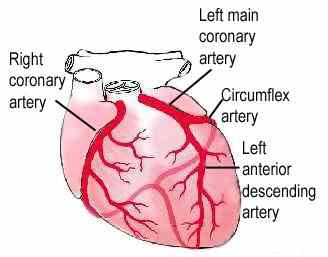
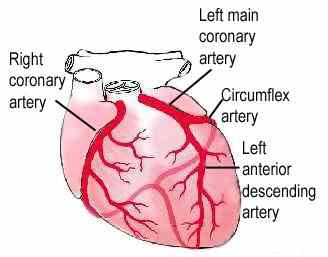
Coronary artery disease is a
narrowing or blockage of the coronary arteries, the arteries that provide the
heart muscle with blood. When the blood flow is slowed the heart doesn't get
enough oxygen and nutrients. This usually results in chest pain called angina.
When one or more of the coronary arteries are completely blocked, the result is
a heart attack (injury to the heart muscle).
What
causes the coronary arteries to narrow?
Coronary arteries become narrowed or
clogged by plaque build-up in the artery walls. Plaque is made of excessive
cholesterol and other substances floating through your bloodstream, such as
inflammatory cells, proteins and calcium. Over time, the inside of the arteries
develop plaques of different sizes. Many of the plaque deposits are hard on the
outside and soft on the inside. The hard surface can crack or tear, exposing
the soft, fatty inside. When this happens, platelets (disc-shaped particles in
the blood that aid clotting) come to the area, and blood clots form around the
plaque. The artery narrows further and, in turn, less room for blood to flow
through the arteries. Plaque build-up in the arteries is called atherosclerosis
(atha-row-skla-row-sis), also known as "hardening of the arteries."
What should you do if
you have coronary heart disease?
When you have coronary artery disease, it is important to take care of your
heart. This is especially true if you have had an interventional procedure or
surgery to improve blood flow to the heart. Procedures do not cure coronary
artery disease. It is up to you to take steps to stop the disease from
progressing.
1. Know the symptoms for
coronary artery disease
The symptoms for coronary
artery disease include:
- Chest discomfort (described as numbness,
heaviness, dull aching, or burning; may radiate to left shoulder, arms
neck, back or jaw)
- Shortness of breath
- Palpitations (a fluttering feeling, skipped
beats)
- Faster heart rate
- Dizziness
- Nausea
- Extreme weakness
Call your doctor if symptoms become more frequent or severe.
Call for emergency assistance if rest and/or medications do
not relieve symptoms within 15 minutes. DO NOT WAIT TO GET HELP.
2. Reduce your risk factors
Medical research has helped
identify certain conditions, called risk factors, which place people at
increased risk for heart disease.
Non-modifiable risk
factors (those that cannot be changed)
- Male
- Older age - Heart disease is more likely to
occur, as you get older.
- Family history (including race)
Modifiable risk factors
(those you can control)
- Cigarette smoking
- High blood cholesterol
- High blood pressure
- Uncontrolled diabetes
- Physical inactivity
- Obesity or overweight
- Uncontrolled stress or anger
- Diet high in saturated fat and cholesterol
- Drinking too much alcohol
If you have more than two of the risk factors
listed, you should discuss your risk factors with your doctor. Your goal is to
decrease your risk factors and lessen your risk for future heart disease
events. This is true if you do not have heart or blood vessel disease, if you
are being treated medically for heart or blood vessel disease, or you have
undergone a procedure (angioplasty, stents, bypass surgery) for heart or blood
vessel disease.
3. Take your medications
Medications are used to control your symptoms and help your
heart work more efficiently. Follow your doctor's instructions when you take
your medications.
It is important to know:
- The names of your medications
- What they are for
- How often and at what times to take your medications
Keep a list of your
medications and bring them to each of your doctor visits. If you have questions
about your medications, ask your doctor or pharmacist.
4. Have procedures or surgery – if necessary
Invasive procedures (such as balloon angioplasty or stents)
or coronary artery bypass surgery may be needed to treat your narrowed or
blocked artery. These procedures
increase blood supply to your heart but they are not a cure for coronary artery
disease. You will still need to focus
on reducing your risk factors to prevent future disease development or
progression. If these procedures are or
have been necessary, your cardiologist or surgeon will discuss the specific
procedure with you.
5. See your cardiologist for regular visits
Schedule regular appointments with your cardiologist (even
if you have no symptoms). Your appointments may be spaced once a year, or more
often, if your doctor feels you need to be followed more closely. Your
appointments should include a medical exam and diagnostic studies (such as an
electrocardiogram).
Call your doctor sooner if your symptoms worsen or become more severe or
frequent.
The Cleveland Clinic Heart
Center cardiologists and surgeons specialize in the treatment of coronary
artery disease. The team approach at
the Cleveland Clinic Heart Center insures that patients receive the best care
before, during and after their procedure. 
Compliments of the Cleveland Clinic Heart Center
|
 Historical Web Sites
Historical Web Sites